Stress, Blood Sugar, and Diabetes

Understanding the intricate relationship between stress and blood sugar levels is vital for effective diabetes management. This article sheds light on how stress hormones impact our physiology, offering crucial insights for those navigating diabetes.
What You Will Learn
- Elevated cortisol levels disrupt insulin sensitivity, making blood sugar control more difficult.
- Acute stress can cause temporary spikes in blood sugar, while chronic stress leads to sustained high levels.
- Behavioral changes during stress can negatively affect medication adherence and healthy lifestyle choices.
- Addressing emotional stress is crucial for managing diabetes and preventing complications.
- Integrating stress management techniques can significantly improve glycemic control.
The Interplay of Stress Hormones and Diabetes Management
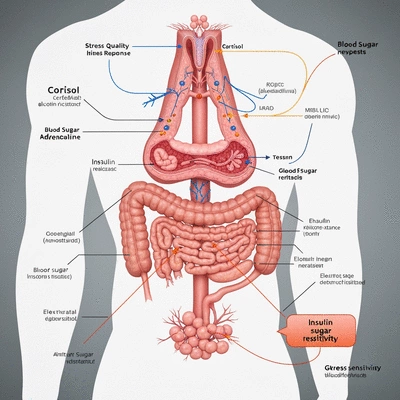
Understanding how different stress hormones affect blood sugar levels and insulin sensitivity is crucial for effective diabetes control. The visual below outlines their distinct roles.
Stress Impact on Blood Sugar: Key Hormones
Cortisol:
Increases glucose production in the liver, reduces insulin sensitivity.
Adrenaline/Norepinephrine:
Triggers glucose release for 'fight or flight' response.
Acute vs. Chronic Stress
Acute Stress:
Temporary spikes in blood sugar.
Chronic Stress:
Sustained high blood sugar, increased diabetes risk, worsens insulin resistance.
Proactive Stress Management Strategies
- Mindfulness/Meditation
- Regular Exercise
- Consistent Sleep
- Balanced Diet
Understanding the Connection Between Stress and Blood Sugar Levels
Stress is more than just a mental hurdle—it has real physiological effects on our bodies, especially regarding blood sugar levels. One of the key players in this process is cortisol, a hormone released during stressful situations. When we face stress, our body triggers the release of both cortisol and adrenaline, which can significantly affect insulin sensitivity and glucose metabolism. For more detailed insights into this connection, refer to information from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
When cortisol levels rise, our body becomes less responsive to insulin, making it harder for glucose to enter our cells. This disruption can lead to elevated blood sugar levels, which is particularly concerning for individuals managing diabetes. Understanding this connection is crucial for effective diabetes management.
Exploring the Physiological Impact of Stress on Blood Sugar
- Cortisol and Blood Sugar Regulation: Elevated cortisol can raise blood sugar levels by encouraging glucose production in the liver.
- Adrenaline's Role: This hormone can trigger a 'fight or flight' response, leading to a surge in glucose in the bloodstream.
- Insulin Sensitivity: Chronic stress can diminish how well our bodies respond to insulin, worsening diabetes management.
In essence, understanding how these stress hormones interact with our metabolism is vital. It sheds light on why managing stress is just as important as monitoring blood sugar levels for anyone dealing with diabetes.
The Role of Acute and Chronic Stress in Diabetes Management
Stress can be classified into two main types: acute and chronic. Acute stress is short-term, often a reaction to immediate threats or challenges. In contrast, chronic stress lasts for an extended period, affecting health over time. Both types impact blood sugar levels, but in different ways. Acute stress may cause a temporary spike in blood sugar, while chronic stress can lead to sustained high levels, increasing the risk of developing diabetes. Research further elucidates how stress impacts diabetes management, highlighting the importance of distinguishing between these types of stress.
Understanding the difference can help you identify your stress triggers. This awareness is a key part of managing diabetes effectively. By recognizing when you are under acute or chronic stress, you can implement strategies to mitigate these effects.
How Stress Hormones Influence Glycemic Control
Cortisol isn't the only stress hormone that affects blood glucose levels. Other hormones like norepinephrine and epinephrine also play a role in glycemic control. When we are stressed, these hormones can cause our bodies to release glucose into the bloodstream, resulting in higher blood sugar levels.
Moreover, prolonged exposure to these stress hormones can lead to metabolic syndrome, a cluster of conditions that increases the risk of heart disease and diabetes. Therefore, recognizing how stress hormones affect our bodies is crucial for anyone managing diabetes. It allows us to adopt effective strategies for stress management and ultimately improve our health.
The Vicious Cycle: Stress, Metabolism, and Diabetes
How Stress Can Worsen Insulin Resistance
Stress and insulin resistance are intricately linked. Psychological stress can exacerbate insulin resistance, making it even more challenging to manage diabetes. When we are stressed, our bodies respond by releasing hormones that interfere with insulin's effectiveness. This can create a vicious cycle, where increased blood sugar levels lead to more stress, further worsening insulin resistance. For a deeper understanding of this cycle, consider reviewing studies on psychological stress and insulin resistance.
Recognizing this cycle is the first step in breaking it. Strategies that focus on stress reduction can significantly improve insulin sensitivity and overall blood sugar control.

Behavioral Impacts of Stress on Diabetes Control
Stress doesn’t just affect our bodies physically; it can also alter our behaviors. When under stress, many people may neglect their medication, make poor dietary choices, or skip exercise. This can lead to poorer blood sugar management and overall health outcomes. It’s important to identify these behavioral changes and find ways to counteract them.
- Medication Adherence: Stress can lead to forgetfulness or reluctance to take medications as prescribed.
- Lifestyle Choices: Stress may drive individuals to choose comfort foods that are often high in sugar and fat.
- Exercise Regimens: High stress levels can reduce motivation to maintain physical activity routines.
By recognizing these impacts, you can take actionable steps to maintain your diabetes management plan, even during stressful times.
The Connection Between Emotional Stress and Health Outcomes
Emotional stress, such as anxiety and depression, can have profound effects on diabetes management. High levels of emotional stress can exacerbate diabetes complications and influence blood glucose levels negatively. It's critical to address these emotional factors as part of an integrated approach to managing diabetes.
For many, finding support through community resources or therapy can provide the necessary tools to cope with emotional stress. Remember, you're not alone in this journey toward better health!
Pro Tip
To effectively manage stress and its impact on blood sugar levels, consider incorporating mindfulness techniques into your daily routine. Simple practices such as deep breathing, meditation, or even a short walk in nature can help reduce cortisol levels and improve your overall well-being.
Frequently Asked Questions About Stress and Blood Sugar
How does stress directly affect blood sugar levels?
Stress triggers the release of hormones like cortisol and adrenaline. These hormones increase glucose production in the liver and can make the body less sensitive to insulin, leading to elevated blood sugar levels.
What is the difference between acute and chronic stress in terms of blood sugar?
Acute stress is short-term and can cause temporary spikes in blood sugar. Chronic stress, lasting for extended periods, can lead to persistently high blood sugar levels, worsen insulin resistance, and increase the risk of developing diabetes.
Can stress impact my diabetes medication adherence?
Yes, stress can negatively impact medication adherence. Individuals under stress may become forgetful or less motivated to take their medications as prescribed, leading to poorer blood sugar control.
What are some effective stress management techniques for individuals with diabetes?
Effective stress management techniques include mindfulness and meditation, regular physical exercise, maintaining a consistent sleep routine, and eating a balanced diet. These practices can help reduce cortisol levels and improve glycemic control.
Why is addressing emotional stress important for diabetes management?
Emotional stress, such as anxiety and depression, can significantly influence blood glucose levels and exacerbate diabetes complications. Addressing these emotional factors through support or therapy is crucial for an integrated and effective diabetes management plan.
Summarizing the Impact of Stress on Blood Sugar and Diabetes Control
Understanding the impact of stress on blood sugar and diabetes control is crucial for anyone managing this condition. Throughout our discussions, we explored how stress hormones like cortisol and adrenaline can disrupt insulin sensitivity, leading to elevated blood glucose levels. We also examined the difference between acute and chronic stress, with each having unique effects on diabetes risk and management.
Additionally, we highlighted how stress influences both behavioral factors—like medication adherence and lifestyle choices—and physiological processes that contribute to insulin resistance. By recognizing these connections, we can take valuable steps toward improving our diabetes management.
- Stress hormones can disrupt glucose metabolism.
- Acute stress may cause temporary spikes in blood sugar.
- Chronic stress can lead to long-term insulin resistance.
- Behavioral impacts include reduced adherence to treatment plans.
In summary, a comprehensive understanding of how stress interrelates with diabetes empowers individuals to take control of their health. By addressing both the physiological and behavioral aspects of stress, we can develop effective strategies for managing blood sugar levels.
Encouraging Proactive Stress Management for Better Diabetes Outcomes
Integrating stress management into diabetes care plans is essential for achieving better health outcomes. As someone who is passionate about empowering individuals with knowledge, I encourage you to adopt the stress-reduction strategies we've discussed. Techniques such as mindfulness, regular exercise, and relaxation practices not only help manage stress but also support effective diabetes control.
It's important to remember that managing stress is not merely an afterthought; it's a vital component of your overall diabetes management plan. By proactively addressing stress, you're not only improving your mental health but also potentially stabilizing your blood sugar levels.
- Practice mindfulness or meditation regularly.
- Engage in physical activities, like walking or yoga.
- Establish a consistent sleep routine.
- Maintain a balanced diet to support overall well-being.
Call to Action: Taking Steps Toward Better Health
Now it’s your turn! I invite you to share your experiences and tips on managing stress and how it has influenced your diabetes control. Every story is unique, and together, we can create a supportive community that inspires and motivates others on their health journeys. Remember, every small step counts, and by taking action today, you can make a significant difference in your health tomorrow!
Recap of Key Points
Here is a quick recap of the important points discussed in the article:
- Impact of Stress Hormones: Stress hormones like cortisol and adrenaline significantly disrupt insulin sensitivity and glucose metabolism.
- Types of Stress: Acute stress leads to temporary blood sugar spikes, while chronic stress can cause sustained high levels and worsen insulin resistance.
- Behavioral Changes: Stress can lead to poor medication adherence, unhealthy dietary choices, and decreased physical activity, impacting diabetes management.
- Addressing Emotional Stress: Emotional factors such as anxiety and depression must be addressed to improve overall diabetes management.
- Proactive Stress Management: Techniques like mindfulness, regular exercise, and a balanced diet are vital for effective diabetes control.









